My Bowel Endometriosis Story: How I Finally Got a Diagnosis
In this article, I share my bowel endometriosis story and how I finally got a diagnosis after years of pain. There are many of us with bowel endometriosis stories and as you read, I hope you feel solidarity from someone else who’s been through the struggle, too.
A few years ago, I was waking up from a diagnostic laparoscopy surgery between the starchy sheets of a Michigan hospital bed. Above the overwhelming nausea and the muzzy anaesthesia brain, I was given my results: endometriosis. Specifically, adhesions and bowel endometriosis.
Endometriosis is a chronic illness: There is no cure, and it is progressive. Doctors don’t know exactly what causes it. But what was the feeling that came over me when I heard the verdict? Relief.
“If you desire healing, let yourself fall ill.”
-Rumi
I searched for answers to my symptoms for so long – years really, but in the months leading up to my first endometriosis surgery, I treated my search for a diagnosis like a full time job.
I had needles poked in my back and barium enemas and X-rays and radioactive pills and allergic reactions and ridiculously restrictive diets and at one point, a literal balloon stuck up my bum (this is called a manometry… it wasn’t fun).
I had to drive long distances for medical appointments at specialist facilities like the University of Michigan Taubmann Center – scratch that, I had to have family drive me because I wasn’t in any shape to get myself home after the procedures.
So to get a diagnosis, an answer, even an incurable one? I can work with that.

What is Endometriosis?
Before I go into my personal health journey and bowel endometriosis story, you should know a little bit about the condition. It will be easy to keep this section brief, because not nearly enough research has been done on endometriosis (despite roughly the same number of people having it as have diabetes).
Endometriosis occurs when tissue similar to the tissue that lines the uterus grows outside the uterus. This causes chronic inflammation, internal bleeding, irritation, autoimmunity, estrogen dominance, and more.
Symptoms can include intense pelvic pain, radiating nerve pain, heavy and painful periods, diarrhea, constipation, painful bowel movements, chronic fatigue, migraines, nausea, infertility, and so much more.
The only way to diagnose endo is through surgery, and although there are ways to treat its symptoms, it cannot be cured.
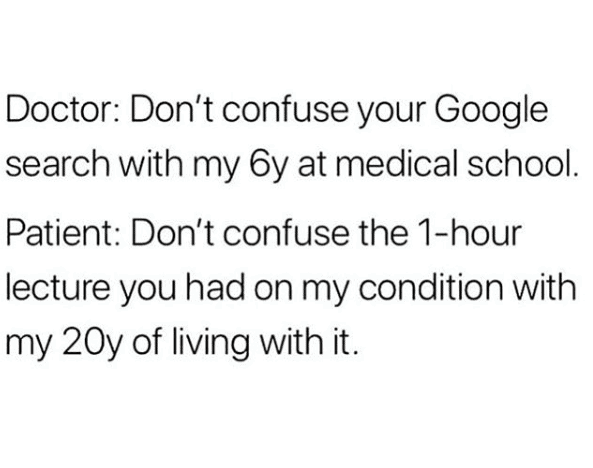
One in 10 people born with a uterus have endometriosis. Yet the utter lack of awareness and research on it could be why it takes on average 7-10 years to get a correct diagnosis. (I have a lot to say about that figure in relation to the patriarchy of the medical system and how women’s bodies have been medicalized historically #ThanksForNothingFreud)
RELATED | Traveling with Endometriosis: Advice From 7 Endo Warriors
How I got Diagnosed with Bowel Endometriosis
Grab yourself a cup of tea or coffee and sit down for a long story, friends.
‘Are you sure it isn’t in your head?’
‘Just drink more water.’
‘Well nothing showed up on your tests so you must be fine.’
‘It’s just IBS. Everyone has that.’
These are just a few things I heard (and said to myself) before my diagnosis. And I cannot portray how painful each of them is when you are truly suffering, but unable to find an answer to why you are suffering. Are you making it all up?
One thing that helped me cope with this isolation and frustration is sharing my health journey on my blog and on Instagram, which is why I’m writing this today – I hope I can give some solidarity and insight to others going through something similar.
I have struggled with my health since a young age, but after my doctor told me I had celiac disease in 2012, and I went on a strict gluten free diet, many of my symptoms dissipated.
Unfortunately four years later, I started developing new digestive symptoms.
My primary symptom was constipation: I experienced constipation for 7-12 days at a time, for months in a row. This caused me so much emotional distress.
It also caused me internal bleeding, bleeding and pain with bowel movements, chronic fatigue, lower abdominal pain, nerve pain shooting into my legs, bloating, distention, acne, anemia, vitamin deficiencies, memory loss, and more.
I didn’t even consider tracking my symptoms alongside my cycle, because that was so irregular (sometimes being on my period for over a month at a time).
I feel that it is very important to mention that this was all very difficult to deal with as someone in her early 20s.
Unfortunately, I went from a girl who loved to travel, take risks, adventure, do yoga and run, and yes to go out partying and dancing with friends. To go from this energetic person to someone who could only eat one bite before bloating up like a 9-month pregnant person, or having one pint of cider on a night out and spending the rest of the night in pain and miserable, suffering the consequences for days afterward… it was horrible.

The Search for a Diagnosis: Irritable Bull…I Mean Bowel Syndrome
Naturally, on my search for a diagnosis, I was focused on my digestive system and so were my doctors. However both my colonoscopy and Sitz Marker Test came back mostly normal, ruling out Crohns, Colitis, and Chronic Intestinal Pseudo Obstruction.
As a result, my gastroenterologist told me I had Irritable Bowel Syndrome (IBS). IBS is the worst kind of diagnosis. It is a diagnosis of exclusion… basically, if your doctor can’t easily figure out what’s wrong with you, they throw you in this ‘waste basket’ diagnosis.
Two people can have IBS but have completely different pathologies and therefore different diseases. It felt like my doctors were giving up on me because my case wasn’t easy for them to solve.
Nevertheless… there are definitely some proven treatments for IBS, so this is what I turned to. First, under a dietitian’s guidance, I did the Low FODMAP diet, a miracle for those with IBS. My constipation and other symptoms only got worse.
Then my gastroenterologist cycled me through three IBS-C medications (Linzess, Trulance, and Amitiza). These are all extremely strong IBS medications yet they had no effect on me even at their highest dosages (apart from Amitiza, which gave me an allergic reaction).
At this point I went back to my gastroenterologist, crying for help. I couldn’t possibly have IBS if nothing for IBS helped me, could I?!
Nothing so far had done anything for my symptoms and they were getting worse. I was so tired I could hardly stand my part time job, and even though I was living with my parents I was exhausted each day.
Everything I ate caused me bloating and constipation. My pain was never my “main” symptom but I started having these intense lower abdominal pains, that is best described as a particularly spiky sea urchin slowly rolling through my organs.
Onto the Gastroenterology Specialists…
Out of her depth, my local gastroenterologist referred me to the specialists at University of Michigan, one of the very best gastro centers in the USA.
It was here that I had my manometry and defecography diagnostic procedures. These (painful, invasive) tests found that I had diminished pelvic muscle tone, and a rectocele (a prolapse of the colon typically due to childbirth or, in my case, chronic constipation).
I went back to my local gastroenterologist with these findings, wondering why do I have a rectocele? Why do I have low muscle tone?
These just seemed like further symptoms of a larger problem, and not a solution in and of themselves. All my gastroenterologist did was refer me to pelvic physical therapy, and warn me that if physical therapy didn’t work, then we would go ahead with the bowel resectioning… AKA chopping off part of my intestines.
This was probably the lowest point of my entire journey. I cannot tell you how many doctors parking lots I sat in my car in, sobbing. Often, I felt like nobody wanted to get to the bottom of my problems, they just wanted to drug me up or chop up my insides.
I began to wonder if I was really sick? Was this all in my head? Based on how sick I felt, shouldn’t my doctors be taking my concerns more seriously? I was hopeless and felt like I was the only one fighting for my health, and I was too exhausted to continue.

A Good Doctor Changes Everything…
It was around this time that a miracle happened. My normal primary care doctor retired and I got a new one in the same practice, Dr. Liz.
Dr. Liz is the best primary care doctor I’ve ever had. She is open minded, she listens, and above all she advocates for me. Really, isn’t this what the role of any doctor should be? Yet I’d never experienced that until I met her.
I should probably mention at this point that through this whole journey, I was completely aware of endometriosis. My mother and grandmother both had severe endo.
Sometimes when I mention this to people now, they ask me “why didn’t you ask about this sooner? Why didn’t you do anything?”. This attitude of shaming and blaming the patient (me, in this case!) is hugely problematic, but so common when it comes to endometriosis.
To explain why it took so long for endometriosis to come up, though, I’ll explain. I was trying to solve digestive problems, not reproductive problems.
Much of the media and gynecologists’ limited education on endometriosis consists of “it’s just a bad period.” This is what I thought endo was. And because (at that point) I didn’t have the horrible periods typical of endometriosis, I didn’t consider it for years.
I figured that I’d deal with endometriosis when and if I ever wanted to have children, because another thing endometriosis is often reduced to is its symptom of infertility.
I did mention endometriosis to my gastroenterologist once and they just said “yeah but we would have found that during the colonoscopy” and brushed it off (which, I’ve learned…. this is SO not true! Endo grows outside organs, not in them. The only endometriosis that would show up in a colonoscopy is deep infiltrating endometriosis at an extremely advanced stage).
When IBS is Actually Endometriosis…
Faced with the prospect of a bowel resectioning, I turned to my friend Google Scholar.
Having stumbled across the article “Endometriosis and irritable bowel syndrome: a dilemma for the gynaecologist and gastroenterologist.” I think my jaw actually dropped. I did another quick search which led me to this speech by Dr. Ken Sinervo at an Endometriosis Foundation conference called “When IBS is Really Endometriosis on the Bowel.”
Bolstered by my findings, I went into Dr. Liz. I presented my theory to her, the fact endometriosis runs in my family, and asked her to help me.
If my gastroenterologist was considering resectioning my bowel, then at the very least I deserved to have one final thing investigated, right?
From here, everything went very fast. Dr. Liz not only agreed my theory was worth investigating, but she personally went to a gynecologist in her practice and argued my case to her. I think this made a huge difference in my journey because, unfortunately, most doctors are more likely to listen to each other than to their patients.
A week later, I walked into my OB/GYN appointment and was told the only way to diagnose endo was via surgery. Forty minutes later, I was scheduled for a diagnostic laparoscopy surgery in five day’s time.
My final diagnosis of bowel endometriosis
The surgery confirmed that I do have endometriosis – but it’s more complicated than that (as I’ve learned, things usually are with endometriosis). In addition to endometriosis implants, my intestines were, in my surgeon’s words, ‘massive and inflamed.’ They also found adhesions.
Adhesions are membranous scar-like tissue that grow due to inflammation, injury, or infection. They are very common for people with endometriosis because the endometriosis itself irritates the surrounding tissue.
My surgery revealed that both my ascending and descending colons were completely wrapped in adhesions, both constricting them and ‘gluing’ them to my inner abdominal wall. The surgeons removed the adhesions, freeing my intestines.
My OB/GYN explained all of this (along with photos, that I will refrain from posting on the internet) at my post-op appointment. She said she had no idea if the endometriosis was causing my digestive symptoms and only time could tell.
At the point of that appointment, nine days post-op, I was still drugged up on painkillers, in pain, and couldn’t tell any difference besides the fact I had two new holes on my belly.
The only thing I knew for sure was I had a diagnosis: endometriosis.
RELATED | My Journey With Endometriosis

How I’m Doing Now: 4 Years Post-Diagnosis
This whole post was very emotional for me to write – to relive the struggle and the frustration and the hopelessness. But perhaps even more emotional is for me is to look back on the months and years since my diagnosis.
In the years since I first wrote this post (just six weeks after my diagnostic surgery), this article has become one of the most popular on Endless Distances. Thousands of endo warriors have discovered it and felt connection through my story, and I am so grateful to provide that.
Through it all, I have kept this article updated as my journey with endometriosis was far from over with my diagnosis. In fact, diagnosis was just the beginning. Below you can read updates from my recovery from diagnostic surgery, all the way to my cross-country journey to the Center for Endometriosis Care for my life changing excision surgery.
Six weeks post diagnosis: Feeling Amazing
At six weeks post op, I felt good.
About two weeks post-op I noticed something: I wasn’t in pain. And I don’t mean operation-related pain.
I realized that I had been living with every day pain for I don’t know how long, and it only took not having it to realize it had been there in the first place. I had grown so resigned to my daily pains that I didn’t even consider them my primary symptom.
As for my primary symptom? My stomach was no longer bloated after everything I ate, things were ‘flowing smoothly’ so to speak. I could go to work and actually have leftover energy to function afterwards.
I wrote this six weeks post-op, when I originally published this blog post:
“Each day that goes by, I am more and more sure that endometriosis was the key in a locked door I have been running at head-on for years on end.
I am honestly tearing up as I write this. It has only been six weeks of this optimal health, but already I am afraid it won’t be forever. I know endometriosis is an incurable, progressive condition.
Although my adhesions and endo implants were removed during surgery, they will likely return. I just hope I can be one of the lucky people to experience years of health before a second surgery is required.
Endometriosis is something I will be dealing with for the rest of my life and I want to learn how to live that life well, and alongside it, instead of against it.”
Six months post op: Everest Base Camp
I became more familiar with my endo symptoms, what a flare felt like, and what triggered a flare. Overall, I felt so much better than I had for years before my diagnosis. I attended a weekly pelvic physical therapy session and was fully committed to it. I slowly got back into exercising because I’d set myself a goal…
Six months after waking up in the hospital bed with my endometriosis diagnosis, I hiked to Everest Base Camp in Nepal!
This was a hugely emotional experience for me, looking back on how far my body had come in such a short time. Before my surgery, getting out of bed was challenging – not to mention high altitude trekking! I began seeing my body, and the pain I’d experienced, in a positive light for the strengths it had given me.
Unfortunately, that’s not the end of the story.
RELATED | 9 Tips That Help Me Survive Travel with Endometriosis
1.5 Years Post Op: The Endo Returned Even Worse
I first updated this blog post in 2020 as it had become very popular, and unfortunately around this time my symptoms returned and my journey with endometriosis took a turn for the worse.
Sadly, as we know, endometriosis is a chronic illness – meaning there is no cure. Just one year after my endometriosis surgery I began experiencing health set backs that I believed were due to recurring endometriosis.
What I learned is that the type of surgery I had, called ablation, was an outdated form where the endometriosis lesions are burned off rather than cut out. The gold standard of endometriosis treatment is excision, a type of surgery where the endo is cut out from the root.
With excision, there is an extremely low recurrence rate and people can usually avoid the stories of multiple painful endo surgeries in their lifetime. Unfortunately, only very specialized gynecologists can perform this surgery.
I learned this information after joining Nancy’s Nook Endometriosis Education, which is a group on Facebook. I would encourage you, too, to join this group and read up on all the materials there.
2 Years Post Op: The Search an Excision Specialist
At this point, I went through the long and difficult process of finding an excision specialist to perform my next endometriosis surgery. I did not want another failed surgery.
As you can probably tell if you read the whole post above, I had a lot of medical trauma from all the invasive procedures and gaslighting I experienced. So the process of finding an excision specialist – which took me to three surgeons, and involved a seven-month surgery waitlist only for my chosen surgeon to retire, beginning the search from scratch, and finally deciding to make the expensive leap for the Center for Endometriosis Care in Atlanta, Georgia – was essentially an experience of re-traumatization.
But I pushed through this trauma because I could not emotionally or mentally handle my life continuing to revolve around endometriosis and the endless painful symptoms that worsened every day.
RELATED | My Journey With Endometriosis
3 Years Post Op: My Second Endometriosis Surgery
Just shy of three years after my diagnostic laparoscopy, I flew with my parents to Atlanta, Georgia for a life-changing excision surgery with Dr. Arrington of the world-renowned Center for Endometriosis Care.
During that surgery I once again had endometriosis found on my bowels: in my sigmoid colon, rectum, rectovaginal space, and appendix. I even had my appendix removed because it was riddled with endo. In addition, endo was found other places including my bladder, uterus, and sidewalls.
I don’t believe this endometriosis grew back since my diagnostic surgery. I (and my surgeon) believe it was there the whole time and was just missed in my first surgery.
I’ve written more about my experience at the CEC in this article about preparing for surgery at the CEC, and this article about what to expect on the day of surgery.
4 Years Post Op: One Year in Endometriosis “Remission”
I’m writing this in November 2022, just over one year after my successful excision surgery for bowel endometriosis, and four years since my diagnostic surgery when I first published this post.
I am SO HAPPY to say that (at least so far) this second surgery was a success. I am completely endo symptom free for the first time in years, and I feel like a different person.
I truly believe that if I hadn’t had this surgery with Dr. Arrington, I would still be suffering with endometriosis to the point that I would be disabled, unemployed, and very physically as well as mentally unwell.
Instead, today I’m fulfilling a lifelong dream of traveling the world full-time with my partner. Before we left for our trip, I drove across the USA twice, and worked as an occupational therapist in two states (a very demanding, physical job that I struggled deeply with due to endometriosis). All in the one year since surgery.
Having bowel endometriosis was the most challenging thing of my life, and it changed so much about me. But one thing I’ve learned is to always fight for myself, trust my gut, and live life to the fullest because our quality of life is not guaranteed.
RELATED | How to Prepare for Endometriosis Surgery

Moving Forward: What’s Next for My Health and Endometriosis Journey?
A diagnosis is just the first step in a long health journey. Although endo cannot be cured, there are ways to treat and manage its symptoms. Surgery and removal of endo is obviously the first step (and preferably, this is excision surgery not ablation surgery like what I had).
Monitoring my endometriosis has become a way of life for me. I’ve tried to balance a more natural approach, free of artificial hormones or awful awful drugs like Lupron, with a medical approach such as trialing (safe) medication.
I found this balanced approach helped me tune in to my symptoms and triggers in the early stages, and has helped me identify recurring symptoms over a year later.
Here are some things I did (and do) to manage endometriosis:
- Educated myself in Nancy’s Nook facebook group
- Switched to using Thinx period underwear. Yep, it’s weird at first, but totally improved my experience on my periods. They really work and help my bleeding anxiety a lot. You can use my link for $10 off your first pair.
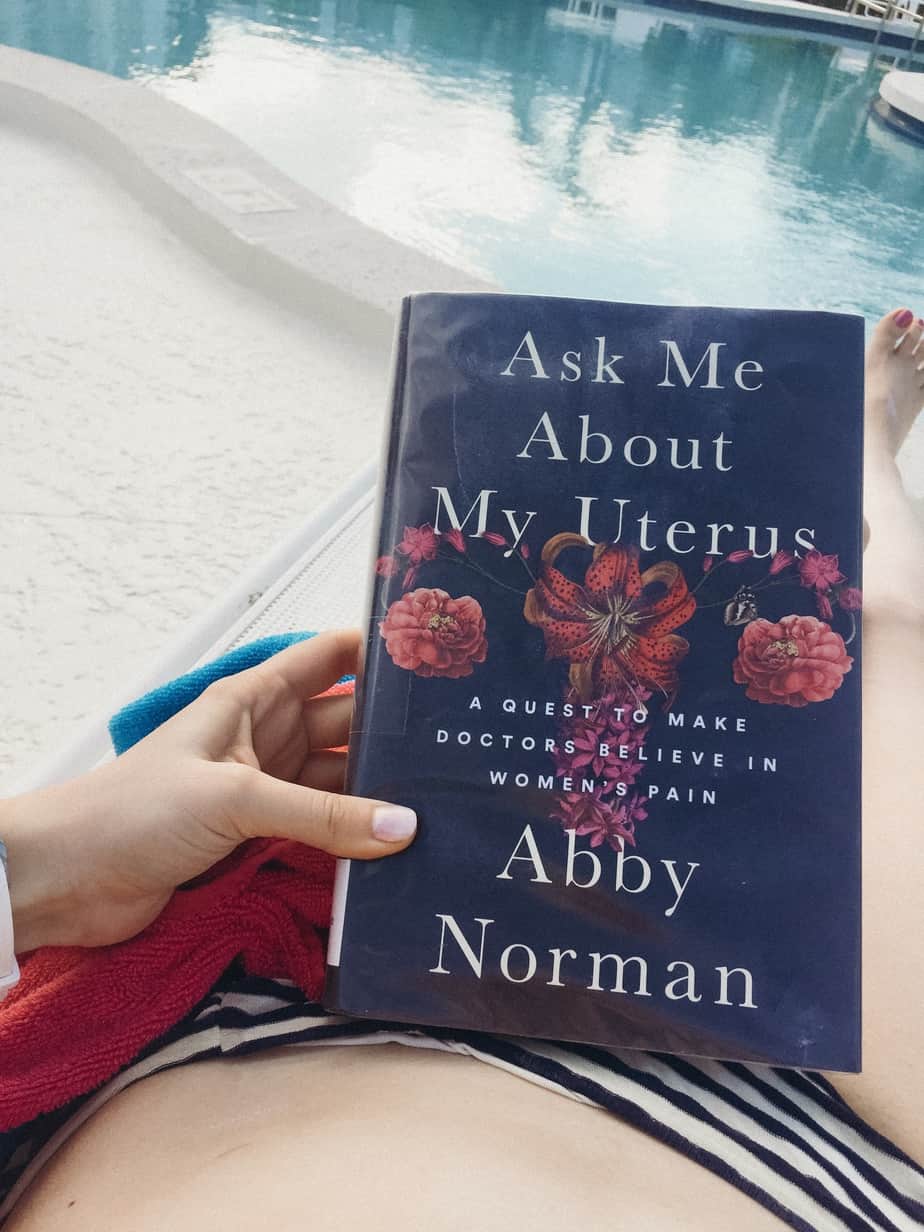
- Read Ask Me About My Uterus a memoir by Abby Norman
- Read Endometriosis Health and Diet Program by Dr. Andrew Cook and adopted some of the philosophies
- Practice yin yoga, hiking, barre, swimming, and other lower impact exercise
- Started taking RainbowLight Women’s One multivitamin to prevent recurring vitamin deficiencies
- Started taking this magnesium citrate powder nightly to help with bowel movements
- Bought an infrared heating pad to help reduce pain when on my period (I like this kind because it’s more portable)
- Committed to pelvic physical therapy
- Practice self myofascial release I learned in physical therapy (I spray this magnesium oil first before massaging my adbomen).
- Trialed muscle relaxant drugs for pain relief (this failed as they made me too sleepy to function!)
- Trialed Motegrity, a new constipation medication, which I currently still take at 2mg. I started this because my digestive symptoms returned.
- Rub Doterra Deep Blue natural pain relief over my abdomen and other painful areas which really helps!
- Give myself permission to rest when I need it
- Biweekly therapy to help cope with the mental health effects of living with chronic illness
The Next Big Step in My Endo Journey:
As I mentioned, sadly since I initially wrote this post my endometriosis symptoms have come back. I am happy to say, though, that as of late 2021 I finally had excision surgery with a “Nook-approved doctor” – Dr. Arrington at the Center for Endometriosis Care. I am waiting a little longer to see my response to surgery, and then I will write a blog post update!
If you join the facebook group I mentioned above, you’ll find a list of approved endo specialist surgeons who can perform excision surgery.
Endometriosis Resources
Before I close, I want to provide some amazing resources on endometriosis that have really helped me on this wild, horrible journey.
Endometriosis research centers
- Nancy’s Nook facebook group – an education-based facebook group with lists of approved excision surgeons
- The Endometriosis Summit – the largest patient and practitioner endometriosis gathering in North America
- Sallie Sarrel Pelvic Physical Therapist – she is a PPT who has endo herself and is an expert on endo care!
- Endo Black – best support and resource group out there for Black women with endo. They have a great facebook group and ambassador community
- Endometriosis UK
- Endo What?
Endometriosis blogs/Instagrams
- Mine is Endless Distances – I share about endometriosis, travel, gluten free food & daily life.
- Endo Girls Blog
- In 16 Years of Endo – she also has an amazing podcast
- Life Above Endo
- Friend with Endo
- Chronically Ill Millenial
- Endo Adeno Warrior
Join in the conversation.
An immense thank you to anyone who has read through this entire post. I tried to shorten it but I also didn’t want to minimize the journey I’ve been on, and that anyone with an undiagnosed chronic illness experiences.
But it’s not just about ME and MY disease though. Having any illness can feel incredibly isolating. Especially if you are traveling which is already a challenge to health. If you have a story to share, please feel welcome to do so in the comments below or on my Instagram.




Thank you for posting your story! This is exactly like my story! I am 2 years post-op and I’m back at the Gastroenterologist again with severe bloating! I’m afraid it’s time for the bowel resection that I refused during the surgery 2 years ago. Will follow you on facebook to see how things are going. Thank YOUUUUUU for sharing!!!!! You are so brave.
Oh no, I hope it doesn’t come to that! And thanks for reading. Have you joined the Nancy’s Nook group on Facebook yet? If not, it has some incredible resources and a list of specialist endometriosis surgeons. Maybe one of them could help you avoid the resection. I’m currently waiting for my surgery with one of them, myself. Best of luck <3
Hi, can you change the link for the Facebook group as it takes you to a crochet page?
Thx
Sorry about that! Link is updated in the post and I’ll also leave it here: https://www.facebook.com/groups/418136991574617
Thanks for posting your story and resources. I wanted to let you know that both links on this page for Nancy’s nook take you to a page not related to endometriosis. I was able to search for the endo one on Facebook but the links here redirected you to a service/products unrelated to endometriosis.
Hi there! My name is Lindsay and I just had my 6th laparoscopic surgery for endometriosis. I live in Michigan and wondering who your surgeon was because I’m really struggling and I might have to get another surgery. I’m not on Nancy’s nook yet. I just really need a good surgeon!!
Thanks for telling your story. I had a total hysterectomy in June and when I was in surgery they found that I had stage 4 endometriosis I had my appendix removed and my rectum had to be repositioned. Now I’m having severe pain and issues with going to the bathroom. I have a CT scheduled for Thursday as my surgeon will not do a colonoscopy with out knowing what he might find as he was called into my hysterectomy to deal with my other issues. I’m scared as I don’t understand the pain why I’m having all this pain as I thought I would be a new person after my surgery which I feel worse.
I want to be like you and persistent with my doctor that what I’m experiencing isn’t normal.
Thanks again
Hi Sarah,
I have never ever commented on a blog post before. In fact, I don’t know if I’ve ever read through an entire blog post until now.
Thank you so much for just putting this out into the world.
I was about to say you have no idea of the journey I have been on… but actually you do.
I have been an inconclusive health journey for almost 2 years now. We’ve been chasing digestive answers, and my issues sound just like your’s (and that’s a first for me). 6-mont pregnant bloating from the second I wake up, to the 9-month bloating when I go to bed. The pain when I eat anything. The constipation. The wild unpredictable periods. I’ve bounced from doctor to doctor to doctor…only for my tests to be clean and my questions to increase. I feel like I have been fighting for anyone to hear me and take my symptoms seriously.
I’ve made it down the rabbit hole of late night researching, and it’s brought me to your story. I have considered endo to be my issue, but now I am almost positive.
Thank you for sharing your journey. I read every word. You have brought me a lot of hope in that perhaps I can put a name to my suffering. Your fight has not been in vain. For once in several years I do not feel alone, and I feel close to answers.
Thank you. I wish you the best of luck on your journey to betterness. I’m a little bit behind you, but I hope t catch up 🙂
This really popped out when looking for information on my adenomyosis, I had a pelvic ultrasound and although not diagnosed by a doctor yet,( because medical help here in the States takes a lifetime.) it reads severe adenomyosis. So I googled it and have been researching it since. Endo sounds a lot like Adenomyosis, but I was trying to link it to my IBS symptoms because I have what feels like severe IBS pain combined with cramps from my period, which gets even worse when I get my period. I’ve been having to live with intense pain for the past 5 months when this thing decided to manifest with unbearable pain in my body, this, after 6 months from January to July of 2020 of continuous heavy bleeding. Anyway, long story short, thanks for sharing. I think I have more insight into what is happening to me as well regarding my bowel problems . It seems that for me a hysterectomy is what will take care of adenomyosis but it’s a major surgery so I’m praying and thinking about it. I hope that you can get the help you need to be better again and enjoy a healthy life! Thanks again for your post!
Thank you for your story. I had an ovary and a fallopian tube removed in 2014 and my surgeon discovered I had significant endo. My half hour of scheduled surgery turned into 4 hours. I had another surgery last year.
Today I experience a new issue and I need to see my doctor. All connected to the bowel and I already know my bowel was troubled with the endo.
What a journey. To all of ladies suffering….keep on keeping on.
Thank you for sharing your story! I was recently diagnosed through an excisional laparoscopy about 3 weeks ago! I was having all sorts of GI issues for months and random nerve pains and fatigue! Eventually the panic attacks and hot flashes took over my life (from the estrogen dominance). They also diagnosed IBS from a colonoscopy and I was literally about to cry talking to a GI specialist. I just happened to be on my period that day in so much pain I barely made it to the appointment, and she was the savior who thought it could be endo! Within 2 months I had the lap done with the Mirena IUD in place as well as an oral birth control to just shut down my ovaries all together. I’m much better but still have some GI issues which could be due to poor gut health and anxiety from all of this. Part of my greatest fear is that this will be a lifelong struggle of daily pain for me. And reading this post, specifically the line about there being a low recurrence with excision surgery, had me tearing up with such relief. So thank you, thank you, THANK YOU for sharing!!! You’re so strong and I hope you can find a better treatment!
Hello I also have Endo and live in Michigan can you please give me the doctor that helped you? Thank you I have been also having all the symptoms you listed.
His name was Dr Hickner out of ann arbor but unfortunately he went on medical leave and decided to retire last week. The search begins from ground zero and his office is recommending only specialist surgeons out-of-state. Once I find a solution for myself I will update this post.
Thank you for your story. Over the years I’ve been looking for answers for our daughter who has lower abdominal pain, digestive flares, loose bm’s, and frequent exhaustion. Her pediatrician suggested IBS… In your search, did you ever come across info about children and endo?
Hi, thanks for reading! I’m sorry for what your daughter is going through. Yes, endometriosis can be found in children. One of the origin theories of endometriosis, which most specialist endometriosis surgeons support, called the mullerian theory of embryogenesis, is that endometriosis is laid down during fetal develeopment. It’s a combination of genetic and environmental factors. So most people who have endometriosis don’t become symptomatic until after their first period, but have the endometriosis as children. And some children do have symptoms. I would recommend joining the Nancy’s Nook Endometriosis Education group on facebook and searching their files for information on endo in children, or asking a question to the group. There are a lot of specialist physicians in that group. Other good resources are https://www.endopaedia.info/ and https://centerforendo.com/
I’m so thankful I found this post, mostly because so many people in my life don’t understand why I won’t break down and take all the meds for my issues. When you said doctors just want to treat things a certain way, I felt that, it’s my experience too. I also remember being dismissed many times about my cramps, until years after having children I noticed that my cramps were contractions and I was missing work. Thank you for being so validating! 🙂 Curious, if you or anyone reading this has mood struggles along with their cycle? Your estrogen comments are making me want to research that point. Just can’t say how excited I am for finding this. So thankful for you and want you to know your suffering is helping others. 🙂
When you said it felt like contractions I’m so amazed you said that because lately that’s how my period cramps feel like!
Hi Sarah, Thank you for your post. I went for a specialist ultra sound a month ago, they found that my endo was stuck on my bowel. And will be having laparoscopy excision of endo and overian cyst tomorrow. I am very anxious and worry as the Dr said they might have to resect my bowel if endo is too stuck. I hope it is not too serious when they open up my tummy tomorrow.
I hope your surgery went well and you are recovering okay!
I just want you to know that I found this blog post right around the time when my symptoms worsened. This post served as a huge insight to me when trying to figure out my own health issues. Every time I questioned my self or was medically gaslighted, I’d come back to this post. A year later, I was diagnosed with endo.
Thanks so much for sharing your story!
And thank you for leaving this kind comment. It actually made me cry a little. I’m so happy I could have a small part in your journey and be there, in a way, for you as you stood up to medical professionals. Congratulations on fighting for yourself.
Currently recovering from Surgery
I also have suffered from “IBS”
Painful periods
Painful passing of gas
Painful trips to the Restroom
I went to the ER with so much pain in all my abdomen. Right away they diagnosed me with appendicitis and was rushed into Surgery, During surgery they see my appendix as normal, but found a “Tumor” inside my Cecum. Had it removed and stitched back my intestines. After pathology the results were Endometriosis.
Now I’m afraid to think that Endometriosis might be hiding somewhere else
Hi Gladys, first of all I’m so sorry that you went through the trauma of emergency surgery. That must have been very difficult for you and you are incredibly strong! Yes, you are right, unfortunately endometriosis tends to occur with multiple lesions and if your emergency surgeon was not an endometriosis specialist (which they almost doubtlessly were not) they likely would not recognize it. It sounds like you may have had deep infiltrating bowel endometriosis. This is usually a sign of more advanced stage III or IV endometriosis that will also have lesions elsewhere in the body. It’s very important to excise ALL endometriosis lesions, as these lesions produce their own estrogen and inflammatory fluids. Even one lesion can cause as much pain as dozens – the research shows no correlation between pain/symptoms and size/amount of lesions. I really want to stress that I am not saying this to scare you, but just to give you some resources so you can get to feeling better. It is a long road to treat endometriosis but diagnosis, which you have, is the first step. I would recommend joining the Nancy’s Nook facebook group and reading the files there to educate yourself on the disease. Check out I Care Better for their list of expert endometriosis surgeons. Try to get your surgical photos and pathology report from your operation. Best of luck with your recovery <3
I think it’s so frustrating going to a doctor with such severe pain and all they can think about is how much they can make off this patient. I deal with severe bladder pain and lower pelvic pain and feels like I’m constantly having a UTI. During my menses, abnormal sized clots about half dollar-golf ball with horrible cramping. I’ve explained all this to a gyn/ob and the only thing he recommended to do was an IUD and call it a day. That’s very frustrating and doesn’t diagnose anything! My mom was diagnosed with endometrial cancer last year and god forbid I have anything like that, but not wanting to get to the bottom of what is exactly going on is very disheartening. My next hope is to try a urologist since I have more options doctor wise because of my health insurance.
Sorry you’re going through that Amanda. In my own experiences I luckily have only once had a doctor (OBGYN) who I thought just wanted to make money off me. Most of the time, sadly, I’ve thought my doctors just didn’t know anything about these diseases beyond a 30 minute lecture they had in med school 20 years ago and no desire to go educate themselves beyond what I personally as their patient can find on Google Scholar. It is sad. There are good doctors out there though, sometimes it takes traveling, and sometimes it is out of network for insurance (check your insurance OON coverage though, I was surprised to find mine pays 80% OON). If you are looking into endometriosis I know that the Center for Endo Care, where I am having surgery next week, has a free records review process. Good luck!
Can you give the link of weighted blanket you use? Please
The one that I use is no longer available online. However I have heard great things about this one by Casper: https://amzn.to/3b8lLbV
I have suffered with endo for quite a while but I wasn’t diagnosed till 2019 when I ended up in the ER thinking I had appendicitis. I had never heard of endo till my obgyn told me I had it. I did so much research that I literally scared myself. In 2019 I had 2 laparoscopies and a colonoscopy which they found nothing. I set up my hysterectomy for early 2020 which I did feel relief for a few months to only have to turn around and have both of my ovaries taken out at different times, and this year 2021 I had to have another laparoscopy which he found just a little. I have tried pelvic floor therapy I have gone to a gasto doctor and which I’m being told is IBS, and finally I am getting into a endo specialist next month! The sad thing is that I am only 28 and all this has happened in 2 years… I still have pain and I’m not sure if it is IBS because I know this pain and I just can’t imagine it is IBS. I hope that this specialist can help me. I really don’t want to go through another surgery if it helps me and not knowing if there is more endo that was possibly missed in the bowls. I want to thank you for your share and I understand so much what you’re going through! I also know what it’s like to not have anybody believe you.
That is so much to go through in a short period of time 🙁 I hope that this new endo specialist can give you the answers and care you deserve! I had my surgery with a specialist at the CEC (Dr Arrington) just about 3 months ago and it was life changing. What a difference a true specialist can make!
I am so thankful that I stumbled upon your story. I have been suffering for years (problems getting pregnant, pain, fatigue, hair loss, etc) and have been on a long journey to get questions answered. Two weeks ago I was diagnosed with Hashimoto’s disease and Fibromyalgia, but still had a question mark lingering about my GI issues. With the Hashimoto’s, I gained weight over a few years and then suddenly lost 40 pounds in 6 months…mainly due to chronic diarrhea (mixed with constipation just for fun). My initial GI diagnosed me with pancreatic insufficiency. I was on meds for that, which made my life miserable. I moved onto another GI who, to be kind, was aloof and uninterested in my issues since I had no glaring abnormal tests. Enter my new GI, whose office I left today with a whole new path..:Endometriosis.
I had an ablation in January, which made me skip my periods, but still have the pelvic pain, painful diarrhea, lower back and shoulder pain, etc. I have an appointment set up with an OB/GYN who specializes in Endometriosis and after doing research, it makes perfect sense.
Thanks for sharing your journey so that others have a sort of syllabus to refer to in our journey.
Cheers
Megan
Thanks for the comment Megan and I’m glad you are finally getting some answers. I’m impressed that it was a GI who suggested endo to you. I feel like not enough GI doctors are aware of endo and think of it as a “gyn only” issue, when really it affects so many of us with GI symptoms! Good luck on the next steps of your journey.
Hi, wow. I am actually sobbing. This sounds EXACTLY like me. I’ve been handed off to four GI specialists and 2 gyn specialists now who can’t figure out what is wrong with me. They labeled me as having IBS, but the problem is literally none of the medications are doing anything. I’ve been on this insane health journey for four years now and it feels like every thing they try comes back normal or not enough to give a diagnoses. I’m struggling so badly. I just had my first appointment with a fertility specialist because all of these health issues are making it hard for my husband and I to get pregnant, and it’s breaking my heart. This literally sounds exactly like me, and I just got told I might have Endo. I feel so lost and confused but this gives me hope that maybe I’m not crazy and it isn’t actually all in my head, but there really is something wrong with me after all. I’m so sick of literally not even being able to hold down a job because I’m sick all the time. I want to be able to eat without fear and live my life without pain every single day.
Thank you for sharing this, and all the resources you’ve used.
So glad you could find some solidarity in my story. Best of luck to you <3
I’ve been struggling with what we think are intestinal problems for an entire year now and it has been awful. Nothing has come up on CT scans, ultrasounds and even colonscopy. My question is did your bowel endometriosis only hurt during your period or get much worse during your period? Just what was the correlation. Thank you
For me, eventually it got to the point I had pain all month long but the “spikes” were worse during my period. There is no one single “normal” experience with bowel endometriosis, though. A lot of people have worse symptoms during their period but that’s not true for everyone. Especially if you’re on any kind of hormonal birth control.
Thank you for sharing your story! It was really validating to hear your experience. I’ve been dealing with pain, GI symptoms, irregular cycles/mood swings for years. I thought my symptoms were all in my head until I finally got a suspected diagnosis of endometriosis. Just curious about the excision surgery… Do you know if you need a diagnostic laparoscopy before getting excision surgery? Ideally I’d like to not go through surgery more than once if it’s not necessary!
No, you don’t! Many people just go straight into the excision surgery with a specialist as a first time if they’ve done their research and suspect endometriosis. You could schedule a consult to get the surgeon’s opinion, too. I wish I could go back in time and only have one surgery, I would’ve saved years of unnecessary pain, so I say go for it.